COLLAPSED DISC
WHAT IS A COLLAPSED DISC?
Whether due to aging, stress, or fluctuations in weight, human spinal discs experience a great deal of stress over the course of their existence.
As time goes on these discs that cushion spinal vertebrae can lose their ability to provide shock absorption, resulting in reduced mobility and pain in the affected patient. One unique presentation of spinal disc deterioration is called a collapsed disc.
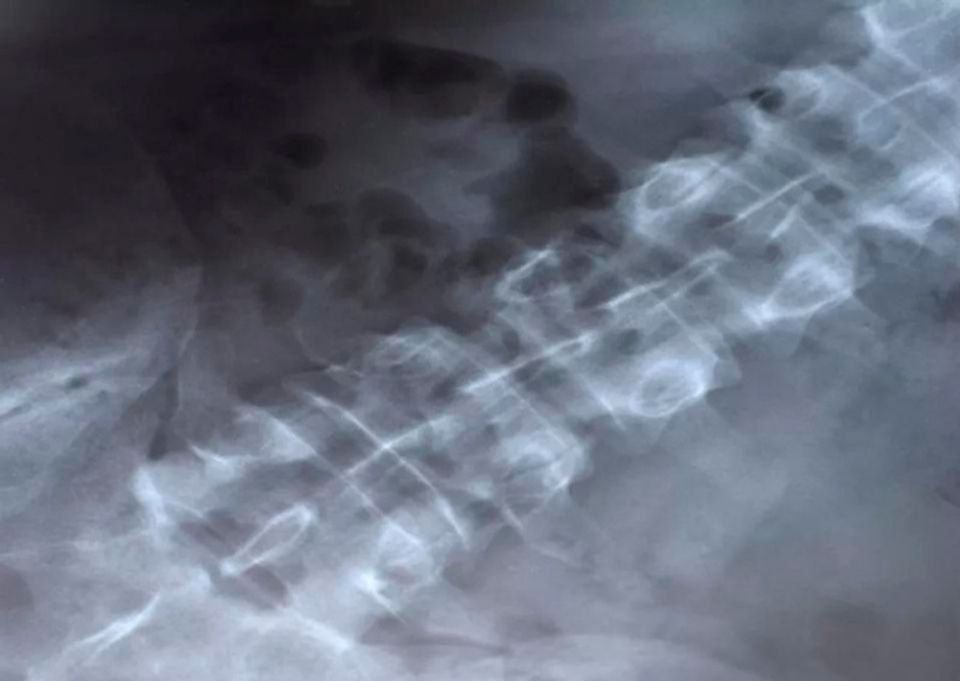
If you were to look at a spine in the standing position – that is, from the back, with a human standing upright – the spinal discs look like rubbery spacers between each spinal bone (vertebrae). Without the presence of these discs, each vertebral bone would chafe against each other.
A disc “collapses” when part of its outer layer, a cartilaginous ring called the annulus fibrosus, loses strength and, subsequently, its original height. The surrounding vertebrae then move closer together, elevating the risk that they will come into contact.
At first, a collapsed disc may not result in any symptoms, particularly if it is not a large “collapse.” Spinal discs naturally deteriorate over time, a process that may or may not be accompanied by pain, tingling, or soreness. But like other spinal maladies, a collapsed disc can be the start of regular back pain, and a far more difficult day-to-day experience for patients. To best understand how collapsed discs occur, what measures can be taken to address the symptoms caused by them, and how to minimize the risk of experiencing this malady, this article will break down the ins and outs of this spinal affliction.
WHAT IS THE DIFFERENCE BETWEEN A COLLAPSED DISC, A HERNIATED DISC, AND A BULGING DISC?
A collapsed disc, like other disc-related maladies like a bulging disc and a herniated disc, can be understood by mapping the relationship between the two core components of natural spinal discs: the previously mentioned annulus fibrosis (the protective outer ring of the disc) and the nucleus pulpous (a jelly- like core inside the ring that provides the flexible layer of cushion between the vertebrae). With each malady, a problem emerges in the relationship between the annulus and the nucleus:
Collapsed disc: The annulus wears down, reducing in height
Bulging disc: The nucleus begins to penetrate the annulus
Herniated disc: The nucleus breaks through the annulus, and begins to press on the parts of the spine outside of the disc, such as the spinal cord itself
In the case of a collapsed disc, the annulus is the primary affected component. Incursion of the nucleus into the area of the annulus could occur, but wear and tear, along with normal aging, can cause the annulus to decrease in strength even without interference from the nucleus. Whatever the source of the collapse, this problem can lead to patient discomfort and pain, and perhaps other spinal struggles down the line.
CAUSES AND SYMPTOMS OF A COLLAPSED DISC
Spinal patients should know that one of the leading causes of disc degeneration in its many forms is something that no doctor will ever find a cure for: the progression of time. As we age, the ordinary wear and tear we put on our bodies causes our discs to slowly lose their original height, strength, and shock absorbing capabilities. Even incredibly active individuals who consume healthy diets, exercise and stretch regularly, and avoid the kind of behaviors that are problematic for spinal wellness could experience disc-related concerns as they age.
However, people can put their spine at greater risk in certain ways. Athletes, as well as those who work in manual labor-centric jobs, face a higher likelihood of disc degenerating owing to the additional stresses they place on their spines while at work.
An additional area of risk is weight. Although bodies are an individual consideration, meaning that there is no one optimal weight that’s right for every single person, it is possible to put on an amount of weight that places burdensome weight loads on our spines. Remember: even the mere act of standing up, without any pronounced exertion, requires muscular exertion, and by extension the carrying of the weight on one’s frame.
The symptoms of a collapsed spinal disc resemble those seen in bulging and herniated discs:
Local pain
Numbness/tingling
Nerve pain
Soreness/sensitivity on the part of the back near to the disc
Muscle weakness
Any of the spine’s three main vertebral areas – cervical (neck), thoracic (mid-back), and lumbar (lower back) – can become afflicted by a collapsed disc, but the lower lumbar area, owing to how much body weight it typically carries, is a common site for disc issues like a collapse.
TREATMENT OPTIONS FOR A COLLAPSED DISC
Like some other disc issues, collapsed discs may not be noticed by patients when they first occur. Not all disc degeneration results in pain, discomfort, or other problems; with normal aging, degeneration is to be expected. It is only once symptoms emerge that a patient can be said to be experiencing degenerative disc disease, or perhaps one of the other bad disc presentations such as a collapse.
Should symptoms begin to appear, however, there should be no immediate cause for serious concern. Although the spine is vital for human muscular and neurological function – it is, after all, the backbone – one need not assume the worst even if a spinal specialist does diagnose a disc problem. Many basic remedies, such as hot/cold treatments and specialized stretches, can ameliorate spinal pain caused by a collapsed disc.
And if the collapse requires some kind of surgical intervention, there are numerous surgical options that follow the philosophy of Minimally Invasive Spinal Surgery (MISS). This approach to spinal surgery involves smaller incisions, more precise surgical movements, and reduced recovery times for patients. These minimally invasive surgeries can even go so far as to replace a disc that has severely degenerated with a new age artificial discs that offer great promise for long-term spine health.
Surgical interventions will depend on each particular patient’s needs and body makeup, so if you find yourself experiencing the kind of spinal and/or back pain that suggests a collapsed disc, consult with your spinal specialist and see about getting scans of your spine to locate the problem before it gets worse.
REQUEST A CONSULTATION
RELATED ARTICLES
DO WEIGHTED NECK PILLOWS HELP WITH NECK PAIN?
As more people look to neck pillows for pain relief, it has raised questions about their effectiveness and safety. Let’s take a look at the potential benefits these pillows can offer along with the limitations for people struggling with chronic neck pain.
WHY DOES MY BACK GET HURT WHEN I GET SICK?
If you've ever had back pain during or after being sick, you're not alone. Here's what might be causing it and how to find relief.